NHS (Mid and South Essex) – Maternity Self-Referral
NHS (Mid and South Essex) – Maternity Self-Referral
NHS (Mid and South Essex) – Maternity Self-Referral
Designing a Resilient, Mobile-First Self-Referral Service for NHS (MSE) Maternity Care
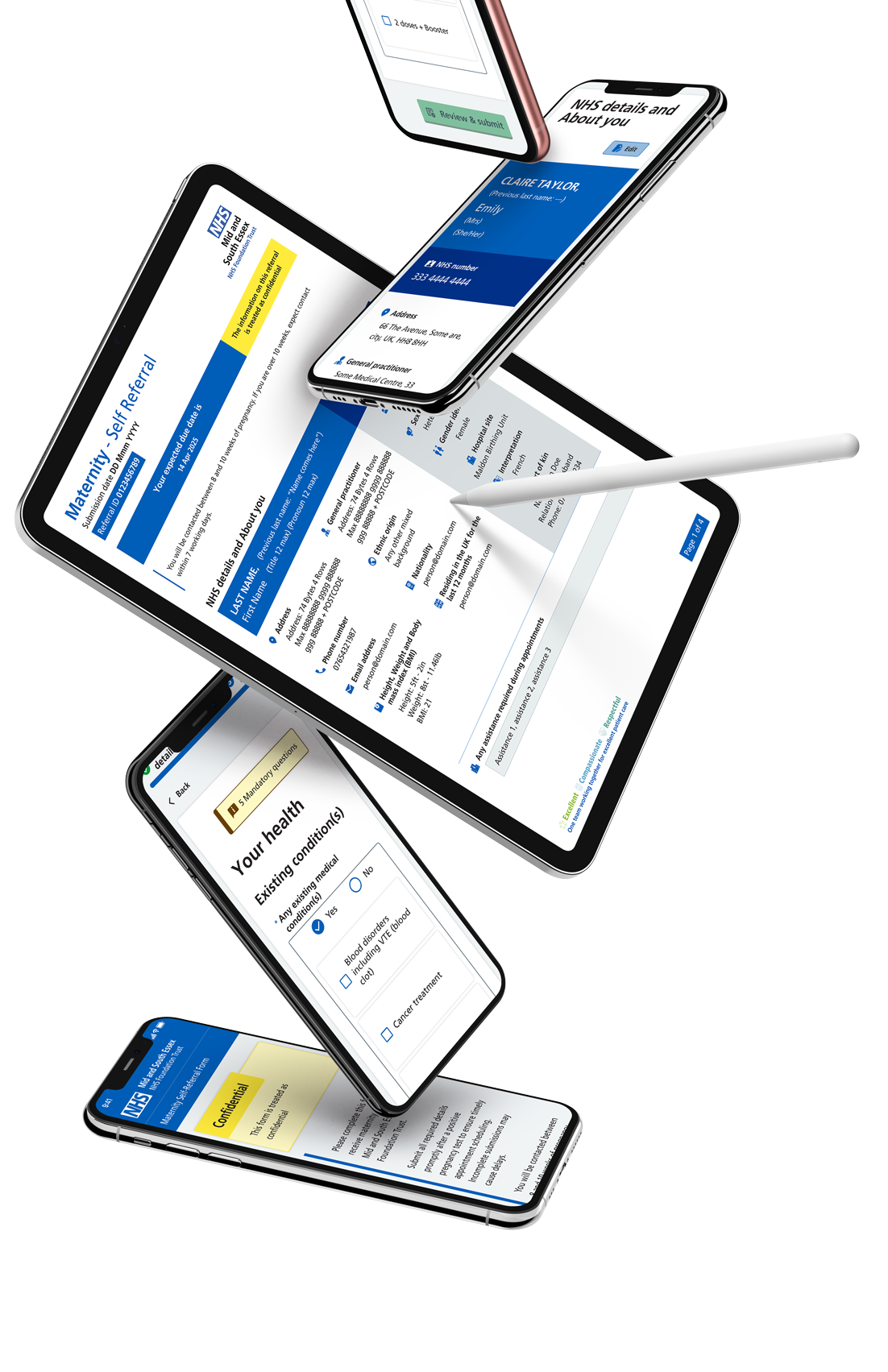
Mobile-First Entry Point & Clinical Data Integrity
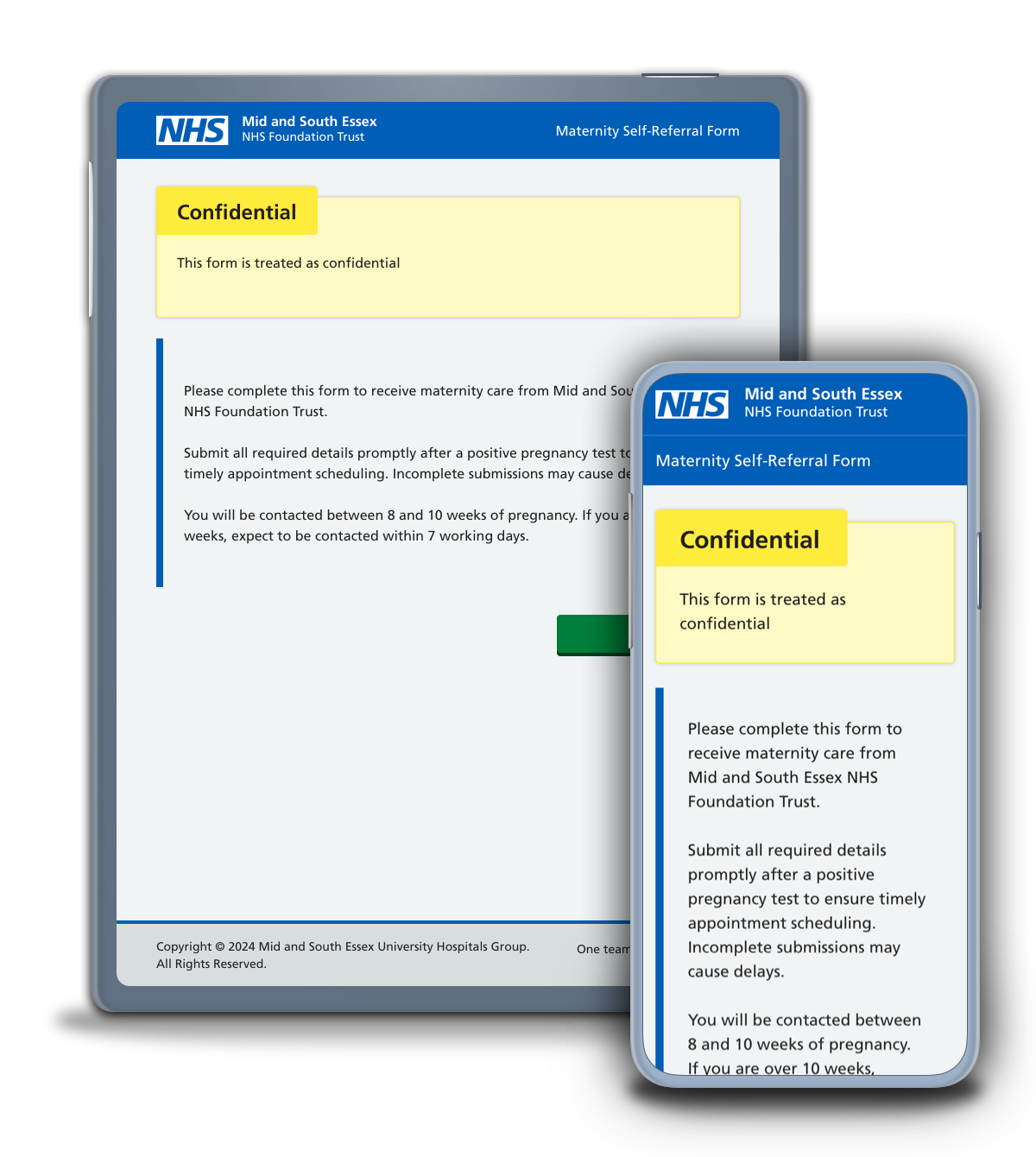
Designing the first step for trust and clarity
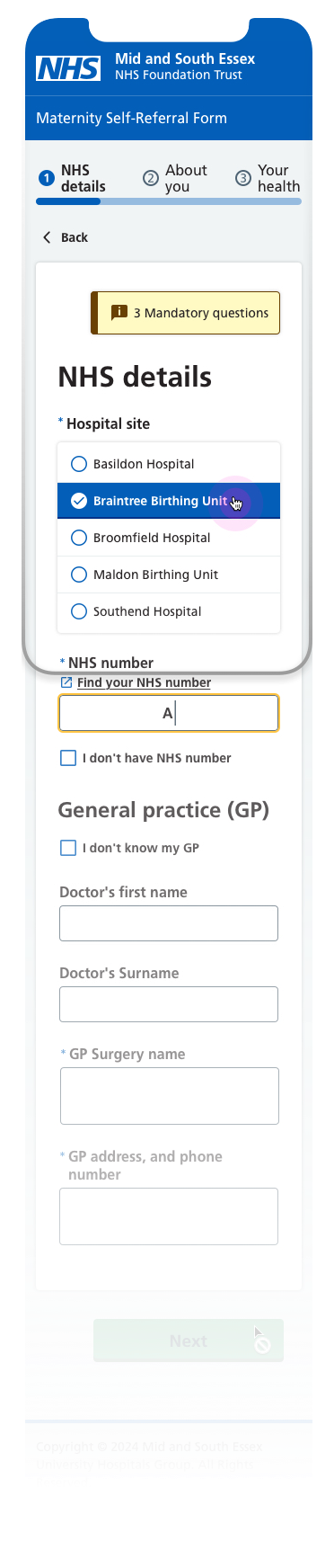
The opening step of the maternity self-referral journey was designed to establish trust while capturing essential NHS and GP information required for safe clinical triage. This screen balances user reassurance with operational needs, setting clear expectations and reinforcing confidence at a sensitive moment in the user journey. Clear headings, familiar NHS patterns, and plain language help users understand what is required and why.
Mobile-first with progressive disclosure
Built mobile-first, the layout prioritises clarity, spacing, and one-handed interaction across small viewports. Information is revealed progressively and grouped logically to reduce cognitive load and prevent form fatigue. The step indicator and consistent navigation provide reassurance and orientation, particularly for users with lower digital confidence, while remaining fully responsive across tablet and desktop.
Inclusive patterns and clinically safe validation
Mandatory logic and inline validation are applied only where clinically required, ensuring the form remains supportive rather than restrictive. Real-world uncertainty, such as users not having immediate access to their NHS number or GP details, is treated as a valid state rather than an error. This approach improves completion rates while ensuring maternity teams receive structured, reliable information suitable for downstream clinical workflows.
Mobile-First Entry Point & Clinical Data Integrity
Designing the first step for trust and clarity
The opening step of the maternity self-referral journey was designed to establish trust while capturing essential NHS and GP information required for safe clinical triage. This screen balances user reassurance with operational needs, setting clear expectations and reinforcing confidence at a sensitive moment in the user journey. Clear headings, familiar NHS patterns, and plain language help users understand what is required and why.
Mobile-first with progressive disclosure
Built mobile-first, the layout prioritises clarity, spacing, and one-handed interaction across small viewports. Information is revealed progressively and grouped logically to reduce cognitive load and prevent form fatigue. The step indicator and consistent navigation provide reassurance and orientation, particularly for users with lower digital confidence, while remaining fully responsive across tablet and desktop.
Inclusive patterns and clinically safe validation
Mandatory logic and inline validation are applied only where clinically required, ensuring the form remains supportive rather than restrictive. Real-world uncertainty, such as users not having immediate access to their NHS number or GP details, is treated as a valid state rather than an error. This approach improves completion rates while ensuring maternity teams receive structured, reliable information suitable for downstream clinical workflows.
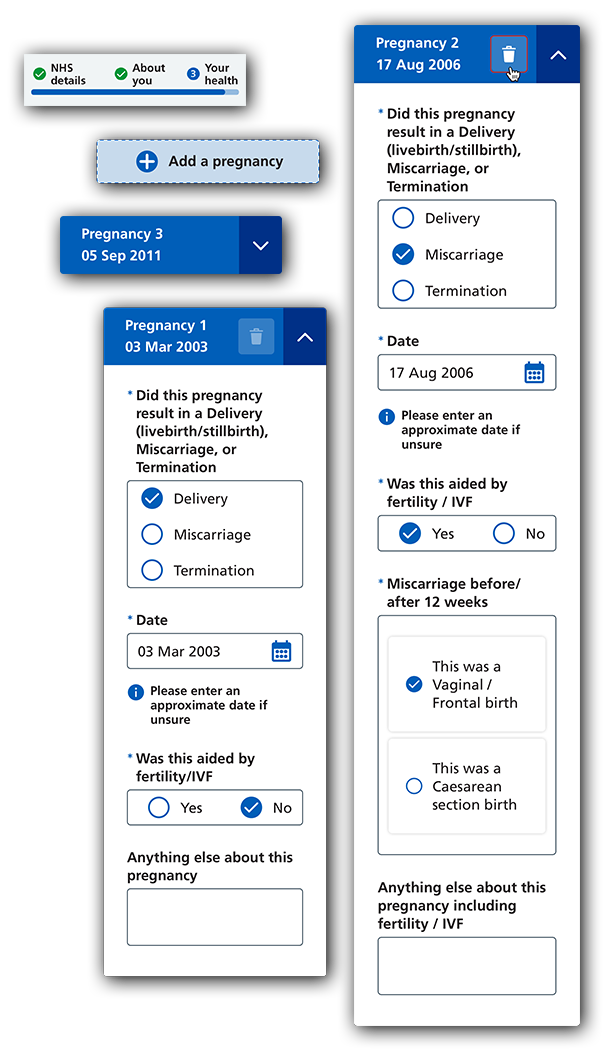
Dynamic Pregnancy History & Conditional Logic
Previous pregnancy history is captured using a dynamic, repeatable pattern that adapts based on user input. Users can add, edit, or remove pregnancy records, with follow-up questions revealed only when clinically relevant, allowing the interface to remain focused and manageable. This approach prevents users from being presented with unnecessary questions while still supporting clinically complex scenarios.
The pattern was designed to accommodate a wide range of obstetric histories, from first-time pregnancies to users with multiple or high-risk previous pregnancies. By structuring information into clear, expandable sections, the experience supports accurate recall and reduces the likelihood of missed or incomplete information. This ensures maternity teams receive a complete and structured view of pregnancy history without increasing cognitive load for the user.
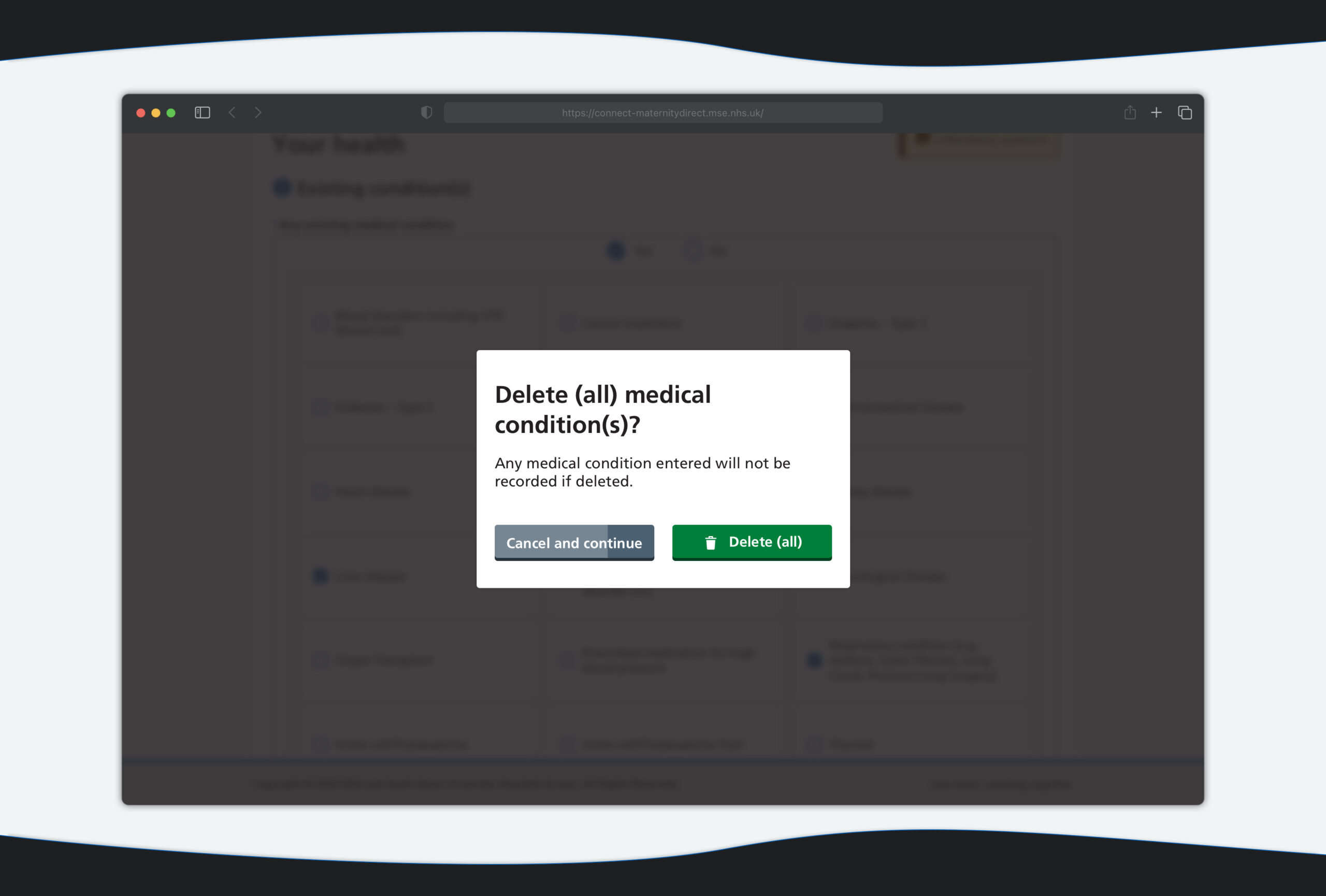
Safety-Critical Actions & Error Prevention
Destructive actions, such as removing a previously entered medical condition, were treated as safety-critical interactions. A clear confirmation modal was introduced to prevent accidental data loss, with plain-English messaging that explains the impact of the action before the user commits. Button hierarchy and wording were carefully designed to support deliberate decision-making while avoiding unnecessary alarm.
Secondary Actions, Recovery Logic & User Protection
A secondary call to action was deliberately introduced alongside the primary destructive action, providing users with a short countdown window to pause or reverse their decision. This recovery pattern recognises that users may act quickly or under stress, particularly when managing sensitive medical information. The countdown logic helps prevent irreversible errors without blocking progress, striking a balance between safety, control, and efficiency.
The interaction was designed to remain accessible and predictable, with clear focus states, visible time feedback, and consistent behaviour across devices. By allowing a brief recovery window, the design reduces the risk of incomplete or incorrect clinical data while maintaining a calm and supportive experience.
Safety-Critical Actions & Error Prevention
Destructive actions, such as removing a previously entered medical condition, were treated as safety-critical interactions. A clear confirmation modal was introduced to prevent accidental data loss, with plain-English messaging that explains the impact of the action before the user commits. Button hierarchy and wording were carefully designed to support deliberate decision-making while avoiding unnecessary alarm.
Secondary Actions, Recovery Logic & User Protection
A secondary call to action was deliberately introduced alongside the primary destructive action, providing users with a short countdown window to pause or reverse their decision. This recovery pattern recognises that users may act quickly or under stress, particularly when managing sensitive medical information. The countdown logic helps prevent irreversible errors without blocking progress, striking a balance between safety, control, and efficiency.
The interaction was designed to remain accessible and predictable, with clear focus states, visible time feedback, and consistent behaviour across devices. By allowing a brief recovery window, the design reduces the risk of incomplete or incorrect clinical data while maintaining a calm and supportive experience.
Clear System States & Submission Feedback
Submission was treated as a critical moment in the journey rather than a passive loading state. Clear, explicit feedback is provided to confirm that the referral is being processed, including visible system messaging and progress indicators. This reassures users that their information has been received and reduces uncertainty at a sensitive point in the experience.
Designing for Resilience & Trust
The submission state was designed to prevent premature navigation, refresh, or duplicate actions while the referral is being generated. Responsive modals adapt across mobile, tablet, and desktop, ensuring consistent behaviour regardless of device. By making system activity visible and predictable, the design builds trust and supports a reliable handover from user input to NHS clinical systems.
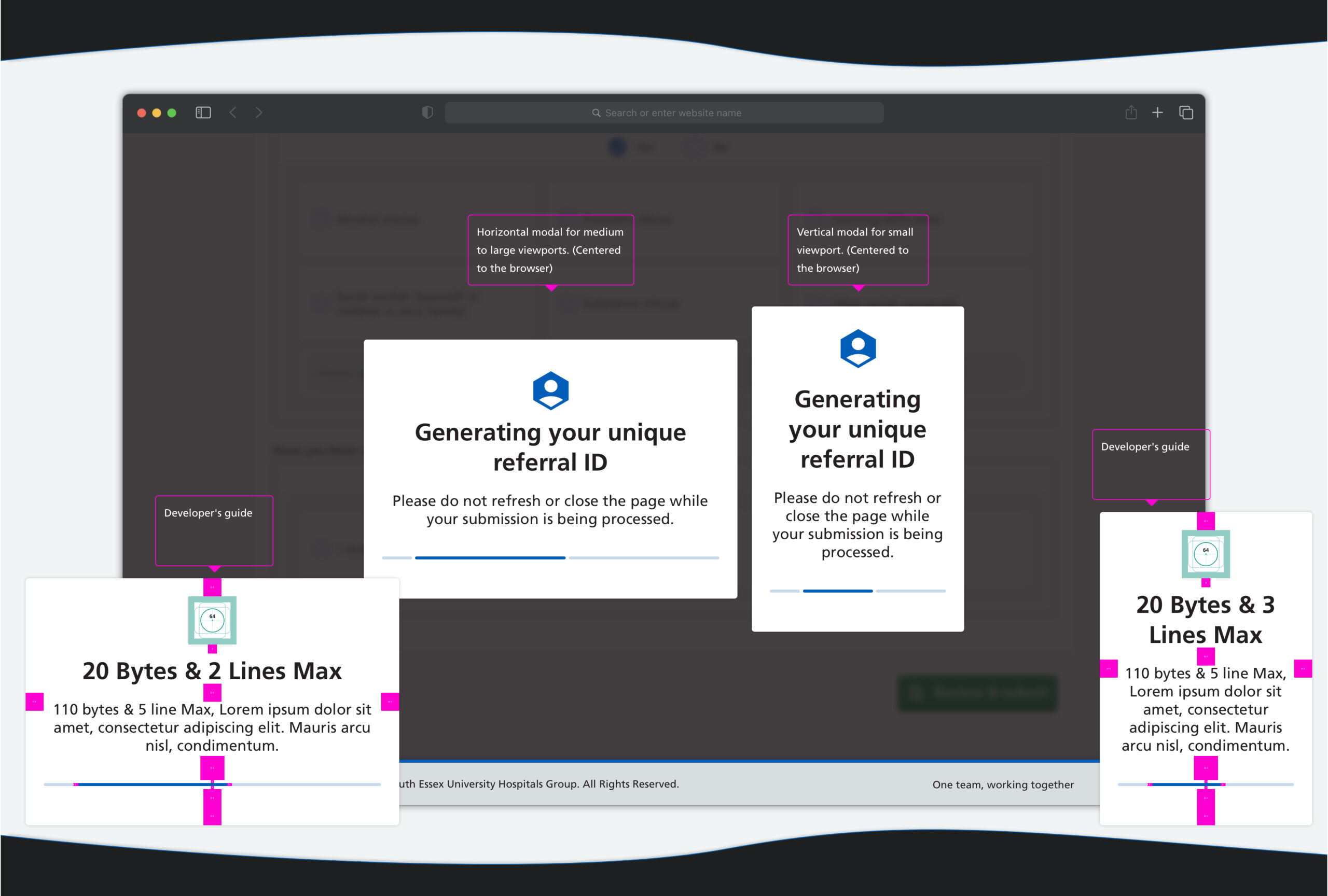
Clear System States & Submission Feedback
Submission was treated as a critical moment in the journey rather than a passive loading state. Clear, explicit feedback is provided to confirm that the referral is being processed, including visible system messaging and progress indicators. This reassures users that their information has been received and reduces uncertainty at a sensitive point in the experience.
Designing for Resilience & Trust
The submission state was designed to prevent premature navigation, refresh, or duplicate actions while the referral is being generated. Responsive modals adapt across mobile, tablet, and desktop, ensuring consistent behaviour regardless of device. By making system activity visible and predictable, the design builds trust and supports a reliable handover from user input to NHS clinical systems.
Outcome & Impact
The redesigned maternity self-referral service significantly improved both user engagement and clinical efficiency. Within two months of launch, completed self-referrals increased fourfold, while direct phone calls to maternity teams were noticeably reduced. Midwives reported receiving more complete and structured information ahead of first contact, allowing appointments to be better prepared and unnecessary follow-ups to be avoided.
By combining mobile-first design, conditional logic, and resilient system states, the service now supports expectant parents with greater confidence while reducing operational strain on maternity teams. The foundation was deliberately designed to scale, with future phases already underway to introduce features such as dark mode, multi-language support, and save-and-return functionality.
These design decisions collectively improved both user confidence and clinical efficiency.Live Service
The maternity self-referral service is publicly available and currently in use. The live form can be accessed below.
For privacy and safety reasons, screenshots shown above do not contain real patient data.
Outcome & Impact
The redesigned maternity self-referral service significantly improved both user engagement and clinical efficiency. Within two months of launch, completed self-referrals increased fourfold, while direct phone calls to maternity teams were noticeably reduced. Midwives reported receiving more complete and structured information ahead of first contact, allowing appointments to be better prepared and unnecessary follow-ups to be avoided.
By combining mobile-first design, conditional logic, and resilient system states, the service now supports expectant parents with greater confidence while reducing operational strain on maternity teams. The foundation was deliberately designed to scale, with future phases already underway to introduce features such as dark mode, multi-language support, and save-and-return functionality.
These design decisions collectively improved both user confidence and clinical efficiency.Live Service
The maternity self-referral service is publicly available and currently in use. The live form can be accessed below.
This project reflects my approach to designing NHS services that balance human needs, clinical safety, and operational reality.
Please note: Content, wording, and functionality may change as the service continues to evolve.









